Innovations médicales & Technologies
The landscape of medical care has transformed dramatically in recent years, with technological breakthroughs reshaping how physicians diagnose, treat, and monitor complex health conditions. From minimally invasive cardiac procedures performed through tiny incisions to artificial intelligence systems that can detect cancers invisible to the human eye, these innovations are fundamentally changing patient outcomes across Canada. For residents of Montreal and beyond, understanding these technologies means making more informed decisions about treatment options and knowing what questions to ask healthcare providers.
This comprehensive resource explores the most significant medical innovations currently transforming healthcare delivery. Whether you’re considering a cardiac intervention, exploring options for chronic pain management, navigating cancer treatment decisions, or simply curious about how robotics and AI are reshaping modern medicine, this overview provides the foundational knowledge you need. Each section breaks down complex technologies into accessible concepts, highlights what patients should know, and addresses both the remarkable benefits and important considerations of these advanced approaches.
Minimally Invasive Cardiac Interventions: Transforming Heart Care
Traditional open-heart surgery, while lifesaving, requires significant recovery time and carries substantial risks. Modern cardiac care has shifted dramatically toward minimally invasive interventions that achieve similar outcomes through small incisions or catheter-based approaches, fundamentally changing the patient experience.
Catheterization and Stent Placement
Cardiac catheterization represents one of the most revolutionary advances in treating coronary artery disease. During this procedure, physicians thread a thin, flexible tube through blood vessels—typically accessed from the wrist or groin—to reach the heart. This approach allows doctors to both diagnose blockages and treat them immediately by placing stents, tiny mesh tubes that prop open narrowed arteries and restore blood flow.
In Montreal, multiple healthcare facilities offer these interventions, with preparation protocols designed to minimize risks. Patients typically undergo blood tests, discuss medications that may need temporary adjustment, and receive detailed instructions about fasting before the procedure. One critical consideration involves contrast dyes used to visualize blood vessels during imaging. While generally safe, these agents can pose risks for individuals with kidney problems or specific allergies, making thorough pre-procedure screening essential.
Recovery timelines have improved dramatically compared to traditional surgery. Most catheterization patients return home within 24 hours, with full recovery taking weeks rather than months. However, post-intervention rehabilitation remains crucial, involving cardiac rehabilitation programs, lifestyle modifications, and ongoing monitoring to prevent recurrence.
Cardiac Ablation and Rhythm Management
For patients experiencing irregular heartbeats, cardiac ablation offers a targeted solution. This procedure uses energy—either radiofrequency heat or cryoablation freezing—to create tiny scars in heart tissue, blocking abnormal electrical signals that cause arrhythmias like atrial fibrillation.
The precision of modern ablation relies heavily on 3D mapping systems that create detailed, real-time visualizations of the heart’s electrical activity. Think of it like GPS navigation for the heart: these systems guide physicians to exact problem areas, improving success rates while minimizing damage to healthy tissue. Before an electrophysiology study, patients undergo similar preparation to standard catheterization, though procedures may last several hours depending on complexity.
The choice between radiofrequency and cryoablation depends on several factors, including the specific arrhythmia type and location. Radiofrequency delivers controlled heat, while cryoablation uses extreme cold—each with distinct advantages in different cardiac regions. Complications remain relatively rare but can include bleeding, blood clots, or damage to blood vessels. Following the procedure, patients require careful monitoring for recurrence, as arrhythmias sometimes return and may necessitate repeat interventions.
Neuromodulation and Advanced CNS Therapies
For individuals living with chronic neurological conditions like multiple sclerosis, Parkinson’s disease, or intractable pain, neuromodulation represents a frontier in treatment—using electrical or chemical signals to modify nervous system activity and restore function or reduce symptoms.
Spinal Cord Stimulation for Chronic Pain
Spinal cord stimulation (SCS) offers hope for patients whose chronic pain hasn’t responded to conventional treatments. This therapy involves implanting a small device that sends electrical pulses to the spinal cord, essentially interrupting pain signals before they reach the brain. Rather than masking pain with medications, SCS modifies how the nervous system processes pain information.
The mechanism relies on the « gate control theory » of pain—imagine a gate that can be partially closed to reduce pain signals traveling to the brain. The implanted stimulator, roughly the size of a stopwatch, sits beneath the skin, typically in the buttock or abdomen, connected to thin wires positioned near the spinal cord. Patients often describe the sensation as a gentle tingling that replaces sharp, burning pain.
Battery life optimization has become a crucial consideration, with modern devices offering rechargeable options that can last a decade or more, compared to non-rechargeable systems requiring replacement every few years. While invasive CNS procedures carry inherent risks—including infection, bleeding, or lead migration—careful patient selection and experienced surgical teams minimize these complications.
Deep Brain Stimulation and Precision Targeting
Deep Brain Stimulation (DBS) takes neuromodulation even further, placing electrodes directly within specific brain regions to treat movement disorders, severe depression, or obsessive-compulsive disorder. Eligibility for DBS involves rigorous evaluation, as this therapy typically serves patients whose symptoms significantly impact quality of life despite optimal medication management.
Beyond electrical approaches, injection therapies for CNS inflammation—such as intrathecal medications delivered directly into spinal fluid—offer targeted treatment for conditions like multiple sclerosis with fewer systemic side effects than oral medications. These advances demonstrate how precision targeting is revolutionizing neurological care.
Precision Oncology and Targeted Therapies
Cancer treatment has evolved from broad-spectrum chemotherapy to increasingly personalized approaches that target specific molecular characteristics of individual tumors, improving effectiveness while often reducing side effects.
Immunotherapy and Targeted Drugs
Recent advances in cancer drugs have introduced therapies that work fundamentally differently than traditional chemotherapy. While conventional treatments kill rapidly dividing cells indiscriminately, newer agents operate through distinct mechanisms:
- Targeted therapies block specific proteins or genetic mutations that fuel cancer growth, attacking malignant cells while largely sparing healthy tissue
- Immunotherapies harness the body’s own immune system, training it to recognize and destroy cancer cells
- Antibody-drug conjugates act like guided missiles, delivering toxic payloads directly to cancer cells via antibodies that recognize tumor markers
Each class produces specific side effects quite different from traditional chemotherapy. Immunotherapies, for instance, can trigger immune-related reactions affecting various organs, while targeted drugs may cause skin changes or digestive issues specific to their molecular targets. Understanding these distinctions helps patients recognize and report symptoms early, enabling timely management.
Navigating Access and Clinical Trials in Canada
Access to innovative cancer drugs in Canada involves complex considerations. While Health Canada approval establishes safety and efficacy, provincial formularies determine public coverage, creating potential delays between approval and accessibility. This reality means some patients face difficult decisions about accessing medications through private insurance, compassionate access programs, or out-of-pocket payment.
The concept of financial toxicity—the financial burden of cancer care—has gained recognition as a legitimate concern affecting treatment decisions and quality of life. Beyond medication costs, patients may face expenses for travel to specialized centers, lost income during treatment, and supportive care needs.
Clinical trials offer another avenue, providing access to cutting-edge therapies before widespread availability. Eligibility criteria vary by trial, typically considering cancer type, stage, prior treatments, and overall health status. Treatment sequencing—the order in which different therapies are used—has become increasingly important, as some sequences prove more effective than others, making specialized oncological expertise invaluable.
Advanced Diagnostic Imaging Technologies
Accurate diagnosis forms the foundation of effective treatment, and imaging technologies have advanced remarkably, enabling physicians to visualize anatomy and pathology with unprecedented clarity.
CT and MRI Innovations
Modern computed tomography (CT) extends far beyond basic X-rays, creating detailed cross-sectional images of the body. Advanced applications include dental 3D imaging that revolutionizes implant planning, and virtual colonoscopy offering a less invasive alternative to traditional colonoscopy for colon cancer screening.
However, these powerful tools require thoughtful application. Radiation exposure from CT scans, while generally safe, accumulates over time, making risk-benefit discussions important, especially for younger patients or those requiring multiple scans. The risk of overdiagnosis—detecting abnormalities that might never cause problems—represents another consideration, potentially leading to unnecessary anxiety and interventions.
Optimizing scan preparation improves image quality and diagnostic accuracy. Depending on the exam, this might involve fasting, drinking contrast material, or temporarily discontinuing certain medications. Following preparation instructions carefully ensures the most informative results possible.
High-Field MRI and the Patient Experience
Magnetic resonance imaging (MRI) uses powerful magnets and radio waves rather than radiation, making it particularly valuable for soft tissue visualization and repeated imaging. High-field MRI systems—those with stronger magnetic fields—provide exceptional image quality, revealing details invisible on standard systems.
In Montreal and across Canada, access to high-field MRI varies between public and private facilities, with wait times sometimes prompting patients to consider private imaging when urgent answers are needed. Public system wait times can range from weeks to months depending on urgency classification, while private clinics typically schedule within days for those able to pay out-of-pocket or with private insurance coverage.
Managing claustrophobia during MRI represents a common challenge, given the enclosed scanner design. Strategies include:
- Open or wide-bore MRI systems that reduce the confined feeling
- Mild sedation when anxiety is severe
- Relaxation techniques, music, or visualization exercises
- Having a family member present in the room when permitted
Contrast agent safety and metal implant compatibility require careful screening. While MRI contrast (typically gadolinium-based) generally poses less kidney risk than CT contrast, patients with severe kidney disease still require precautions. Metal implants need evaluation on a case-by-case basis—many modern implants are MRI-safe, but older devices or certain types may be contraindicated.
Robotic and Minimally Invasive Surgery
Surgical robotics represents perhaps the most visible technological transformation in operating rooms, enabling procedures with precision exceeding human hand capabilities while minimizing tissue trauma.
Robotic-Assisted Procedures
Robotic surgery systems don’t operate autonomously—rather, they translate surgeon movements into ultra-precise micro-movements of specialized instruments. The surgeon sits at a console, viewing a magnified 3D image of the surgical field while controlling robotic arms that eliminate hand tremor and allow movements impossible with conventional instruments.
Precision in microsurgery has improved dramatically. Procedures requiring suturing of tiny blood vessels or nerves, once extraordinarily challenging, become more reproducible with robotic assistance. This technology has expanded applications across specialties, from cardiac surgery to gynecological procedures to cancer operations requiring nerve-sparing techniques.
Training of robotic surgeons follows rigorous protocols, typically involving simulation practice, proctored cases with experienced mentors, and gradual progression to more complex procedures. Institutions offering robotic surgery maintain credentialing requirements ensuring surgeon competency before independent practice.
Benefits, Costs, and Practical Considerations
Robotic-assisted surgery outcomes often demonstrate advantages over traditional approaches:
- Smaller incisions resulting in less pain and scarring
- Reduced blood loss during surgery
- Shorter hospital stays, often same-day discharge for some procedures
- Faster return to normal activities
- Improved precision in delicate anatomical areas
Cost and coverage in Canada varies. While many hospitals have invested in robotic systems, not all procedures qualify for full public coverage, sometimes leaving patients with facility fees or requiring private insurance. The higher upfront costs of robotic systems and longer operating times for complex cases must be weighed against benefits like reduced complications and faster recovery.
The risk of system failure, while rare, necessitates protocols for immediate conversion to conventional techniques if technical problems arise. Hospitals maintain backup plans and ensure surgical teams can complete procedures using traditional methods if needed.
Minimally invasive gynecological and abdominal surgery particularly benefits from robotic assistance. Procedures like hysterectomy, fibroid removal, or endometriosis treatment can often preserve fertility while achieving therapeutic goals. Scar reduction benefits extend beyond cosmetics—smaller incisions mean less tissue disruption, lower infection risk, and reduced adhesion formation that can cause future complications.
Artificial Intelligence in Clinical Practice
Artificial intelligence has moved from theoretical promise to practical reality in healthcare, augmenting physician capabilities and potentially improving diagnostic accuracy and efficiency.
Diagnostic and Predictive Applications
AI in medical screening currently excels at pattern recognition tasks, particularly in radiology and pathology. Machine learning algorithms analyze medical images—mammograms, chest X-rays, retinal scans, skin lesions—often matching or exceeding human expert performance in detecting abnormalities. These systems don’t replace physicians but serve as a « second set of eyes, » flagging potential issues for human review.
Radiology workflow improvement represents one of AI’s most immediate impacts. By prioritizing urgent findings, reducing time spent on routine measurements, and highlighting areas requiring attention, AI enables radiologists to focus expertise where it matters most. In busy emergency departments, predictive analytics help identify patients at highest risk for deterioration, guiding resource allocation and clinical attention.
Think of AI as an extremely knowledgeable assistant that never gets tired or distracted—it can process vast amounts of data instantly, recognize subtle patterns across thousands of cases, and provide decision support based on comprehensive evidence review.
Ethical and Privacy Considerations
Despite impressive capabilities, AI in healthcare raises important concerns requiring ongoing attention. Bias in AI algorithms presents a significant challenge—if training data predominantly represents certain populations, the resulting AI may perform poorly for underrepresented groups, potentially exacerbating healthcare disparities.
The risk of data privacy breaches increases as healthcare systems collect and analyze massive datasets. Canadian privacy regulations, including provincial health information acts, provide frameworks for protecting patient data, but the evolving nature of AI applications requires constant vigilance and updated safeguards.
Optimizing the doctor-AI relationship remains crucial. Technology should enhance rather than replace the human elements of medicine—empathy, contextual understanding, and the ability to weigh complex factors beyond algorithmic analysis. The most successful implementations position AI as a tool supporting physician judgment, not supplanting it, with final decisions remaining firmly in human hands.
As these technologies continue evolving, staying informed empowers patients to engage meaningfully with healthcare providers about options, ask relevant questions, and make decisions aligned with personal values and circumstances. Medical innovation offers tremendous promise, but realizing that promise requires both technological advancement and thoughtful, patient-centered implementation that prioritizes safety, accessibility, and genuine improvement in health outcomes.

AI in Dermatology: Is an App Really as Accurate as a Doctor for Checking a Mole?
Contrary to the hype, an AI app’s accuracy for mole checking is not a simple number; it’s a complex issue deeply affected by hidden biases and the specifics of Canada’s healthcare landscape. AI models often show reduced accuracy on darker…
Lire la suite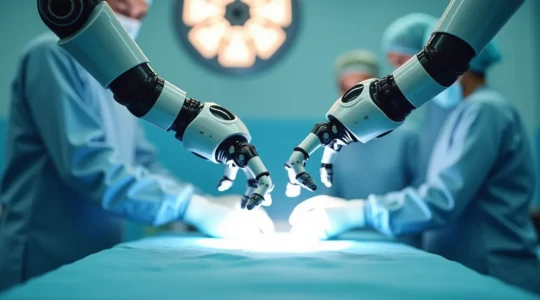
Robotic Laparoscopy for Hysterectomy: Why Is the Recovery 2 Weeks Faster?
The significantly faster recovery from robotic hysterectomy stems from a continuum of care that minimizes the body’s systemic stress before, during, and after the procedure. Superior surgical precision and smaller incisions drastically reduce tissue trauma, inflammation, and blood loss. Pre-operative…
Lire la suite
Da Vinci Robot vs Human Hand: Which Reduces Hospital Stay by 2 Days?
Robotic surgery isn’t just a marginal improvement; it’s a technological leap that translates directly into shorter hospital stays, less pain, and a dramatically faster return to your life. Tremor-filtering technology allows for superhuman precision, protecting delicate nerves and minimizing complications….
Lire la suite
1.5T vs. 3T MRI: Which Machine Should You Choose for Brain Imaging?
The choice between a 1.5T and 3T MRI isn’t about which is « stronger, » but which provides the highest diagnostic yield for your specific neurological question. A 3T MRI offers superior detail (higher signal-to-noise ratio) crucial for complex cases like small…
Lire la suite
3D Mammography vs 2D: Is Tomosynthesis Worth the Extra Private Cost?
For a Montreal woman with dense breasts, the choice between a free 2D mammogram and a paid 3D one isn’t about technology—it’s a strategic decision about managing uncertainty and hidden costs. 3D mammography significantly reduces anxiety-inducing callbacks by pinpointing issues…
Lire la suite
How to Get Coverage for Immunotherapy Treatments Not Listed on RAMQ?
Securing RAMQ coverage for a high-cost, unlisted immunotherapy in Quebec is not a matter of luck, but a systematic process of bureaucratic navigation. You must construct an undeniable clinical file for the « médicament d’exception » program, not simply make a request….
Lire la suite
How Can Neurostimulation Relieve Chronic Pain When Drugs Fail?
Neurostimulation is not a last resort; it’s a proactive strategy to regain control from chronic pain by directly intercepting pain signals before they reach the brain. The process in Quebec involves a clear qualification pathway, from specialist referral to a…
Lire la suite
How Cardiac Ablation Permanently Fixes Your Heart’s Electrical Short-Circuits: An Insider’s View
Cardiac ablation permanently corrects your heart’s electrical system by treating it like a precise engineering project, not just a simple plumbing fix. Advanced 3D mapping creates a detailed « electrical blueprint » of your heart, allowing for pinpoint accuracy. Targeted energy—either heat…
Lire la suite
Angioplasty vs. Bypass: A Montreal Surgeon’s Guide to a Faster Recovery for Active Seniors
For an active Montrealer, the choice between angioplasty and bypass is not about recovery time, but about the quality of your return to performance. Minimally invasive options like drug-eluting stents and radial artery access, standard in leading Montreal centres, dramatically…
Lire la suite