
The choice between a 1.5T and 3T MRI isn’t about which is « stronger, » but which provides the highest diagnostic yield for your specific neurological question.
- A 3T MRI offers superior detail (higher signal-to-noise ratio) crucial for complex cases like small tumours, early-stage multiple sclerosis, or subtle traumatic brain injuries.
- A 1.5T MRI remains the clinical workhorse for many standard brain evaluations and is often more tolerant of patient motion or certain metallic implants.
Recommendation: For complex, undiagnosed neurological symptoms in Montreal, pursuing a 3T scan—even through private options to bypass public system delays—is often a justifiable strategy for achieving definitive diagnostic certainty.
When you’re faced with perplexing neurological symptoms—unexplained dizziness, persistent headaches, or subtle cognitive changes—the goal is a clear diagnosis. Your physician will likely recommend a Magnetic Resonance Imaging (MRI) scan of your brain, but the conversation often stops there. You may not realize that a critical choice exists between different types of MRI machines, primarily the 1.5 Tesla (1.5T) and the 3 Tesla (3T). This isn’t just a technical detail; it’s a fundamental decision that directly impacts the quality and diagnostic power of the images obtained.
The common assumption is that « stronger is always better, » leading many to believe a 3T MRI is the default superior option. While the 3T magnet is twice as powerful, the reality is far more nuanced. The optimal choice depends entirely on the clinical question being asked. For some conditions, a 1.5T provides excellent, clear images. For others, particularly those involving minute structural changes in the brain, the enhanced signal and resolution of a 3T scanner are indispensable for a confident diagnosis. The key is not magnet strength alone, but maximizing the diagnostic yield—the amount of useful clinical information gleaned from the scan.
This guide, from the perspective of a neuroradiologist, will demystify the technology behind 1.5T and 3T MRI. We will explore not only the clinical indications for each but also the practical realities of accessing this technology within Montreal’s unique dual public and private healthcare landscape. We will delve into critical related topics, from managing claustrophobia and understanding contrast agents to the implications of medical implants and the emerging role of artificial intelligence in refining diagnostic accuracy. The objective is to empower you with the knowledge to have a more informed discussion with your healthcare provider about the best imaging strategy for your specific needs.
To navigate this complex topic, this guide breaks down the essential considerations into clear, focused sections. Explore the table of contents below to find the answers to your most pressing questions about advanced brain imaging.
Summary: 1.5T vs. 3T MRI: A Patient’s Guide to Advanced Brain Imaging in Montreal
- Open MRI vs Wide Bore: Which Is Better for Severe Claustrophobia?
- Private MRI in Quebec: Is It Worth $800 to Skip the 6-Month Wait?
- Gadolinium Contrast: Is It Safe for Patients With Kidney Issues?
- The MRI Danger of Hidden Metal Shrapnel or Old Tattoos
- Why You Must Stay Still for 45 Minutes During a High-Def MRI?
- Why Does a « Pacemaker for Pain » Stop Signals Before They Reach the Brain?
- CT Scan Radiation: How Much Is Too Much Within One Year?
- AI in Dermatology: Is an App as Accurate as a Real Doctor for Mole Checking?
Open MRI vs Wide Bore: Which Is Better for Severe Claustrophobia?
For many patients, the primary concern with an MRI isn’t the technology but the experience of being in a confined space. Severe claustrophobia can make a scan unbearable, leading to motion artifacts that render the images undiagnosable. In Montreal, patients have several options to mitigate this anxiety. The traditional MRI has a bore (the tunnel) diameter of about 60cm. A « Wide Bore » MRI, now the standard in most modern private clinics and some hospitals, increases this to 70cm. This extra space significantly reduces the feeling of confinement for most patients without compromising image quality, especially on 1.5T systems.
For the most severe cases of claustrophobia, an « Open MRI » may seem like the ideal solution. These machines are open on the sides, eliminating the tunnel entirely. However, this design comes with a significant trade-off: a much lower magnetic field strength, typically between 0.5T and 0.7T. This results in a lower signal-to-noise ratio, longer scan times, and reduced image resolution. For complex neurological questions, an open MRI often fails to provide the diagnostic yield necessary for a confident assessment. Therefore, a 70cm wide-bore machine, often combined with sedation or relaxation techniques, is almost always the preferred choice for claustrophobic patients requiring high-quality brain imaging.
The table below outlines the key differences between the MRI options available to patients in the Montreal area. As shown, a 3T wide-bore machine, while rare, offers the pinnacle of both comfort and image quality.
| MRI Type | Bore Width | Field Strength | Best For | Montreal Availability |
|---|---|---|---|---|
| Wide Bore | 70cm diameter | 1.5T | High-resolution brain imaging with less confinement | Medvue (Private) |
| Traditional Closed | 60cm diameter | 1.5T-3T | Highest quality images | MUHC, CHUM (Public) |
| Open MRI | Open sides | 0.5T-0.7T | Severe claustrophobia | Limited availability |
| 3T Wide Bore | 70cm diameter | 3T | Best of both worlds | McGill BIC (Research) |
Your Action Plan for Managing MRI Claustrophobia in Quebec
- Ask the clinic: « Do you offer music or video goggles during the scan? »
- Inquire: « What are your sedation options and are they covered by RAMQ if in-hospital? »
- Request: « Can I visit the MRI suite before my appointment to familiarize myself? »
- Confirm: « Is your machine a wide-bore 70cm opening or a traditional 60cm? »
- Prepare: Practice relaxation techniques and consider bringing your own music if the clinic’s policy allows it.
Private MRI in Quebec: Is It Worth $800 to Skip the 6-Month Wait?
The clinical need for a 1.5T or 3T MRI is only half the equation in Quebec; the other half is access. The public healthcare system (RAMQ) covers MRI scans, but patients often face significant delays. For non-urgent cases, wait times can be extensive. A 2024 report highlights the scale of the issue, finding the total wait time from referral by a GP to receiving treatment following an MRI was a median of 28.9 weeks in Quebec, significantly longer than the Canadian average. For a patient with debilitating neurological symptoms, this delay can mean months of uncertainty and anxiety.

This is where Montreal’s private imaging clinics offer a compelling alternative. For a fee, typically ranging from $550 to $800, a patient can often get a scan within days or weeks, not months. While this is a significant out-of-pocket expense, it’s important to consider the total financial picture. According to an analysis of the costs, patients can claim this as a medical expense on both federal and Quebec provincial tax returns. This can result in a tax credit that reduces the net cost by 20-30% or more, depending on your income. The decision, therefore, becomes a trade-off: the certainty and peace of mind of a quick diagnosis versus the financial cost. For many, the ability to either rule out a serious condition or begin treatment promptly is well worth the investment.
Ultimately, the choice to pursue a private MRI is a personal one, weighing the urgency of your clinical situation against your financial capacity. For those with complex symptoms where a 3T scan is recommended for its high diagnostic yield, the private route may be the only feasible way to access this technology in a timely manner, as public 3T scanners are often reserved for the most acute or complex inpatient cases.
Gadolinium Contrast: Is It Safe for Patients With Kidney Issues?
For many neurological MRIs, particularly when investigating tumours, inflammation, or vascular issues, a contrast agent is injected intravenously to enhance the visibility of certain tissues. The most common type is a gadolinium-based contrast agent (GBCA). Gadolinium is a rare earth metal that, on its own, is toxic. In GBCAs, it is chemically bound (chelated) to a molecule that allows it to be safely administered and then filtered out of the body by the kidneys. However, concerns have been raised about its safety, especially for patients with pre-existing kidney disease.
The primary risk, though extremely rare with modern agents, is a condition called Nephrogenic Systemic Fibrosis (NSF), a debilitating disease that can occur in patients with severe kidney dysfunction who are exposed to certain older types of GBCAs. This has led to a crucial distinction between two classes of agents: linear GBCAs and macrocyclic GBCAs. Macrocyclic agents have a more stable chemical structure that « cages » the gadolinium ion more securely, drastically reducing the risk of it being released into the body. As a result, they are considered much safer for all patients, including those with kidney issues. As the FDA has noted in its safety communications, the risk profile differs significantly between agent types. In this context, it is reassuring to know that:
Quebec’s reputable imaging centres exclusively use the newer generation of macrocyclic GBCAs, which have a significantly lower risk profile for patients with kidney issues
– FDA Drug Safety Communication, FDA warnings on gadolinium-based contrast agents
Before any contrast-enhanced MRI, your kidney function will be assessed via a simple blood test (checking creatinine levels to estimate eGFR). If you have a known history of kidney disease, this will be discussed in detail. For the vast majority of patients with normal or even mildly impaired kidney function, the diagnostic benefit of using a modern macrocyclic GBCA far outweighs the minimal risk.
The MRI Danger of Hidden Metal Shrapnel or Old Tattoos
An MRI machine’s powerful magnetic field is its core technology, but it also represents its greatest potential danger. The static magnetic field—always on, even when not scanning—is thousands of times stronger than the Earth’s magnetic field. Any ferromagnetic metal object brought into the scanner room can become a dangerous projectile. This is why screening protocols are so rigorous. However, the danger isn’t just from external objects; it’s also from metal hidden within the body.
Obvious metallic implants like joint replacements or dental work are usually made of non-ferromagnetic materials like titanium and are considered MRI-safe. The real concern lies with unexpected or forgotten metal. A tiny metal fragment from a past workplace injury (e.g., grinding metal) that lodged in or near the eye could be moved by the magnet, causing catastrophic injury. Patients with a history of military service, construction work, or any injury involving projectiles must report it, and a preliminary X-ray may be required to clear them for the scan.
Another often overlooked source of metal is tattoo ink. Older tattoo inks, particularly those with red or black pigments used before the 1990s, could contain iron oxides. When exposed to the MRI’s magnetic fields and radiofrequency pulses, these metallic particles can heat up, potentially causing skin irritation or, in rare cases, first or second-degree burns. This also applies to some forms of permanent makeup or microblading. It is critical to disclose all tattoos to the MRI technologist. While the risk is low with modern inks, the screening process is a non-negotiable safety step. Before any scan in a reputable Montreal facility, you will be required to complete a detailed screening checklist covering these points:
- Complete a detailed safety questionnaire about all implants and past injuries.
- Disclose any tattoos, especially those with red or black ink from the pre-1990s era.
- Report any history of working with metal or military service.
- Inform the technologist about any permanent makeup or microblading.
- Undergo a preliminary X-ray screening if there is any uncertainty about the presence of internal metal fragments.
Why You Must Stay Still for 45 Minutes During a High-Def MRI?
Patients are often surprised by the length of an MRI scan, which can last from 20 to 60 minutes or more for a detailed brain study. The instruction to remain perfectly still is absolute, as even the slightest movement can ruin an image. To understand why, it’s helpful to think of how an MRI creates a picture. Unlike a camera that captures an image instantly, an MRI builds it up piece by piece, line by line, in a virtual space called « k-space. »
The scanner performs multiple acquisitions, called sequences, each designed to highlight different tissue properties (e.g., T1 for anatomy, T2/FLAIR for pathology, DWI for stroke). Each sequence takes several minutes to fill its portion of k-space. If you move during a sequence, the data for that line is recorded in the wrong place, resulting in a blurry or ghosted image, known as a motion artifact. This is particularly critical in high-field 3T MRI. While 3T MRI provides twice the signal strength of a 1.5T machine, which allows for higher resolution images, it is also more sensitive to motion. A tiny movement that might be negligible on a 1.5T scan can create significant artifacts on a 3T scan, negating the benefit of the stronger magnet.
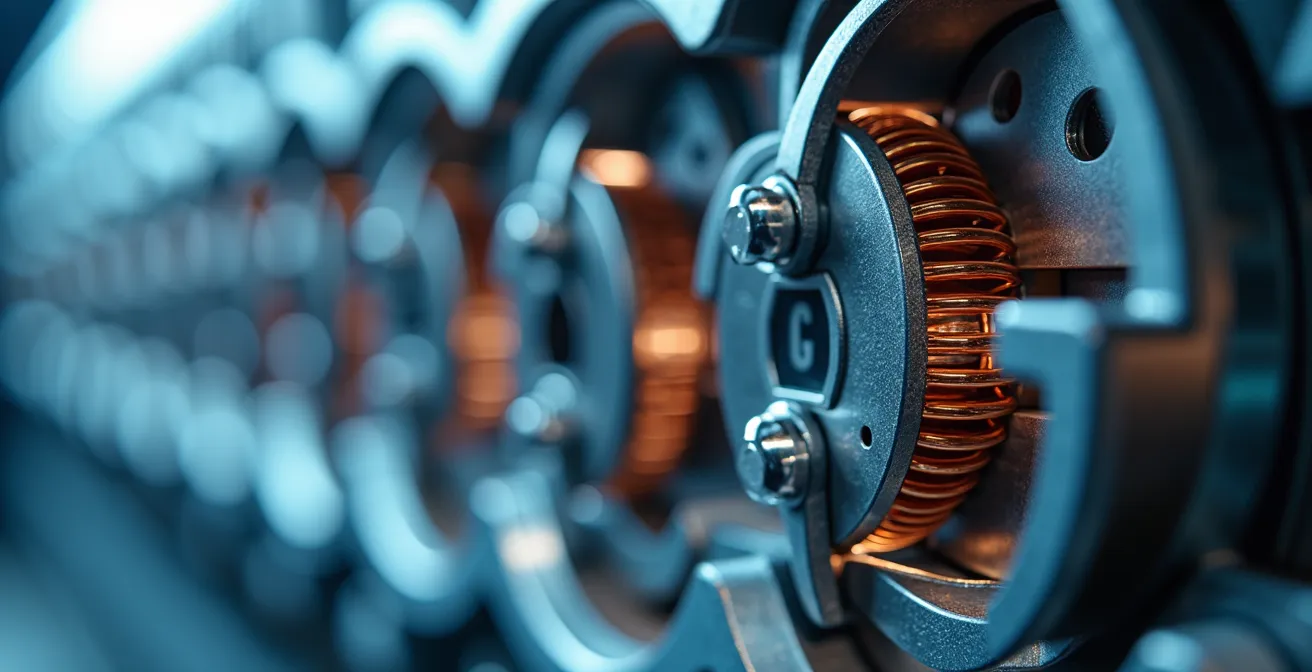
The intricate gradient coils inside the machine (as seen in the image above) are responsible for spatially encoding the signal to build the image. This process requires absolute stability. A single corrupted sequence may need to be repeated, adding more time to the scan. For a patient with a complex neurological issue, where the goal is to detect very small lesions or subtle changes, motion-free, high-resolution 3T images are not just preferable—they are essential for achieving the highest possible diagnostic yield and providing a definitive answer.
Why Does a « Pacemaker for Pain » Stop Signals Before They Reach the Brain?
For patients with certain types of chronic pain, a Spinal Cord Stimulator (SCS)—often called a « pacemaker for pain »—can be a life-changing therapy. This implanted device consists of thin wires (leads) placed near the spinal cord and a small generator (the battery, similar to a cardiac pacemaker) implanted under the skin. It works by delivering tiny electrical impulses that interfere with the pain signals traveling up the spinal cord to the brain. Instead of feeling pain, the patient may feel a gentle tingling sensation (paresthesia) or, with newer devices, no sensation at all.
The presence of an SCS creates a significant challenge for MRI. The device contains metallic components and electronic circuitry that can interact with the MRI’s powerful magnetic and radiofrequency fields. This interaction can potentially lead to device malfunction, movement of the leads, or dangerous heating of the tissue around the implant. For this reason, for many years, patients with an SCS were completely ineligible for MRI scans. However, technology has advanced, and many modern SCS devices are now designated as « MRI-conditional. »
Case Study: SCS Patient Protocol at the Montreal Neurological Institute
At the Montreal Neurological Institute-Hospital, patients with Spinal Cord Stimulators who require a brain MRI follow a strict, multi-disciplinary protocol. This involves close coordination with the patient’s pain clinic to reprogram the device into a safe « MRI mode » or turn it off entirely before the scan. In many cases, a representative from the device manufacturer must be present during the appointment to ensure correct settings are used. Furthermore, a careful risk-benefit analysis is performed to decide if the diagnostic information from a 3T scan is necessary, or if a 1.5T scan is sufficient and safer, as most SCS devices are only conditional for 1.5T field strengths.
This stringent protocol highlights that while MRI is now possible for many SCS patients, it is a highly specialized procedure that must be managed by an experienced team. The decision to proceed, and at what magnetic field strength, is always made on a case-by-case basis, prioritizing patient safety above all else.
CT Scan Radiation: How Much Is Too Much Within One Year?
When a rapid assessment of the brain is needed, particularly in an emergency setting to look for bleeding or a skull fracture, a Computed Tomography (CT) scan is often the first choice. It’s fast, widely available, and excellent for these specific indications. However, its primary drawback is its use of ionizing radiation (X-rays) to create images. While the radiation dose from a single CT scan is low and generally considered safe, the cumulative dose from multiple scans over time is a valid concern for both patients and clinicians.
There is no single « magic number » for how much radiation is too much, as the risk is cumulative over a lifetime. The guiding principle in radiology is ALARA: As Low As Reasonably Achievable. This means using radiation only when the diagnostic benefit clearly outweighs the potential long-term risk. In stark contrast to CT, the NIH confirms that MRI uses zero ionizing radiation. It relies on magnetic fields and radio waves, making it an entirely different and safer modality for repeated imaging or for use in sensitive populations like children and young adults.
Patient Journey: From CT to MRI in the Quebec System
A typical patient journey in Montreal illustrates the complementary roles of these technologies. After a head injury, a patient might arrive at the Jewish General Hospital ER, where a quick CT scan is performed to rule out an acute bleed. This provides immediate, life-saving information. Days or weeks later, if the patient has persistent symptoms like headaches or cognitive fog, their neurologist will refer them for a follow-up 3T MRI. The MRI is used to look for subtle signs of traumatic brain injury (like micro-hemorrhages or axonal injury) that are invisible on CT. This two-step process provides the best of both worlds: the speed of CT in an emergency and the superior soft-tissue detail and safety of MRI for detailed, non-urgent follow-up, avoiding unnecessary additional radiation exposure.
This common clinical pathway underscores why MRI, and particularly high-resolution 3T MRI, has become the gold standard for detailed neurological assessment. It provides unparalleled diagnostic information without the concern of radiation, making it the ideal tool for tracking disease progression or for any situation requiring meticulous evaluation of brain tissue.
Key Takeaways
- For complex neurological questions, a 3T MRI’s superior signal-to-noise ratio provides a higher diagnostic yield than a 1.5T machine, making it the preferred tool for detecting subtle pathology.
- Accessing a timely MRI in Montreal often involves a trade-off: enduring long waits in the public system (RAMQ) or paying out-of-pocket for rapid access through private clinics, a cost that can be partially offset by tax credits.
- Patient safety is paramount. Full disclosure of all medical implants, past injuries involving metal, and even old tattoos is non-negotiable to prevent serious injury from the MRI’s powerful magnetic field.
AI in Dermatology: Is an App as Accurate as a Real Doctor for Mole Checking?
The rise of Artificial Intelligence (AI) is transforming medicine across numerous specialties. In dermatology, for instance, AI-powered smartphone apps claim to be able to analyze pictures of moles and assess their risk of being cancerous. While these tools are becoming more sophisticated, they are not yet a substitute for a dermatologist’s trained eye and a biopsy. However, in the field of radiology, AI is not positioned as a replacement for the expert but as an incredibly powerful assistant, a « second pair of eyes » that enhances diagnostic capabilities.
This is particularly true in neuroradiology, where AI algorithms are being developed to process the vast amounts of data generated by an MRI scan. Montreal is at the very heart of this revolution. The city’s status as a global AI research hub gives local clinicians and patients access to cutting-edge tools. As leading researchers in the city have noted, this local expertise is being directly applied to medical imaging.
Montreal’s status as a global AI hub (Mila) means local research is creating tools that help radiologists detect disease earlier on high-resolution 3T brain scans
– MICA Lab, Montreal Neurological Institute Research
Case Study: AI-Enhanced MRI Analysis at McGill
At the McConnell Brain Imaging Centre at McGill, AI is already in clinical research use. Techniques like « compressed sensing » use AI to reconstruct high-quality images from less data, which can significantly reduce MRI scan times without sacrificing quality. Other AI tools are trained on thousands of annotated 3T brain scans. These algorithms can automatically segment brain structures, measure their volume, or flag tiny, subtle abnormalities that might be at the threshold of human perception. This allows a Montreal neuroradiologist to more efficiently and accurately identify the earliest signs of diseases like Alzheimer’s or multiple sclerosis, ultimately leading to earlier diagnosis and intervention.
Therefore, while an AI app for mole checking remains a screening tool, AI in neuroradiology is a diagnostic enhancement tool. It works in synergy with the 3T scanner’s high-resolution images and the neuroradiologist’s expertise to maximize the diagnostic yield from every scan.
Armed with a deeper understanding of MRI technology and the specific landscape in Montreal, your next step is to have a detailed discussion with your neurologist to determine the optimal imaging pathway for your specific clinical situation and diagnostic needs.
Frequently Asked Questions about 1.5T vs. 3T MRI
What’s the difference between MRI-conditional and MRI-safe devices?
MRI-conditional devices, like many modern pacemakers or spinal cord stimulators, can be scanned but only under a specific set of conditions (e.g., at 1.5T field strength only, with specific software settings). MRI-safe devices, such as titanium hip replacements, are made of non-magnetic materials and pose no known hazards in any MRI environment.
Can I get a 3T brain scan with my spinal cord stimulator?
It is highly unlikely. Most current SCS devices are only conditional for 1.5T MRI scans. A 3T scan would be outside the approved safety parameters and requires special, explicit clearance from both your pain specialist and the device manufacturer, which is rarely granted for routine clinical scans.
What happens during the MRI if I have an SCS?
A strict protocol is followed. Before the scan, the device must be professionally reprogrammed into « MRI mode » or turned off. A representative from the device company may need to be present to verify the settings before you enter the scanner room and to restore normal function after the scan is complete.